Can Scoliosis Cause Herniated Discs?
Scoliosis is a condition that can cause a wide variety of symptoms and effects, including disc herniation. A herniated disc occurs when the inner core of a spinal disc has shifted or pushed outward due to pressure or trauma. Herniated discs can cause intense pain, numbness, and tingling in the arms and legs. In severe cases, it can also lead to a loss of mobility.
Scoliosis may increase the risk of disc herniation. As scoliosis causes the spine to deviate from its normal alignment, it can increase the pressure on spinal discs, leading to an increased risk of possible herniation. As such, if you have scoliosis, there’s a greater chance that you might develop a herniated disc as a direct result.
What Is Scoliosis And What Causes It?
Scoliosis is a condition where the spine curves and rotates to one side, and it can affect people of all ages. It’s a relatively common issue, affecting around 2-3% of adolescents, 10% of adults over 40, and 38 % of adults over 60.
Scoliosis can be caused by various conditions, including neuromuscular diseases, genetic predisposition, spinal injuries or infections, and structural abnormalities. However, it’s worth noting that 80% of scoliosis cases are “idiopathic,” meaning they have no known cause.
Although it is not always a serious condition, scoliosis can cause pain and discomfort in the back, shoulders, hips, and legs. It can also lead to abnormalities in posture, such as the shoulders and hips being higher on one side.
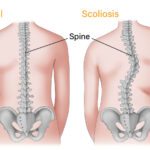
illustration of a spine with scoliosis versus a normal spine
What Is A Herniated Disc, And How Do They Develop?
A herniated disc is an injury to the intervertebral disc, which is an important structure that sits between each vertebra (spinal bone) in the spine. These discs consist of a tough outer layer and a soft inner core. The purpose of the intervertebral discs is to absorb shock and provide additional stability in the spine.
When disc herniation occurs, the inner core of the disc is pushed out through a tear or rupture in the outer layer. As a result, the disc bulges outward and can press against the nerve roots, causing pain, tingling, numbness, and muscle weakness. Several injuries or conditions can lead to a herniated disc, including:
- Overuse of the spine
- Trauma to the spine
- Age-related degeneration
- Poor posture
- Obesity
- Smoking
- Medical conditions such as scoliosis
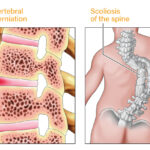
illustration of intervertebral disc herniation and scoliosis of the spine
Risks Factors Of Herniated Discs Caused By Scoliosis
Scoliosis can increase the risk of herniated discs as it alters the normal alignment of the spine. The following outlines the different risk factors that may contribute to the increased risk of disc herniations associated with scoliosis:
- People with scoliosis may have weak abdominal muscles because of the curvature in their spine. Weak abdominal muscles can put extra strain on the back, increasing the risk of herniating a disc.
- Scoliosis can also cause changes in the spinal curvature, leading to an uneven distribution of weight through the discs. This uneven weight distribution can increase the pressure on certain discs and may lead to herniation.
- People with scoliosis often have a limited range of motion in the spine, leading to muscle imbalances and uneven pressure on the discs.
- Exercise and movement are essential to keeping the discs healthy and hydrated. However, some people with scoliosis may be limited in the types of exercise they can do. When the intervertebral discs become dehydrated, they are more prone to herniation.
Does Scoliosis Cause Herniated Discs?
It’s important to understand that disc herniation can happen to anyone, even those without conditions like scoliosis. After all, herniated discs can be caused by various conditions and activities, including a traumatic injury or lifting heavy items with poor technique.
However, scoliosis can increase the risk of herniated discs as it can lead to weakened abdominal muscles, uneven spine curvature, and a limited range of motion in the spine. These issues can cause extra strain on the discs, increasing the risk of herniation.
As such, there is no direct causal link between scoliosis and herniated discs. This means that just because you have scoliosis, it doesn’t necessarily mean you’ll develop a herniated disc. In most cases, there are ways to reduce the risks and prevent herniated discs from occurring.
Can You Prevent Herniated Discs If You Have Scoliosis?
If you have scoliosis, developing a herniated disc is a risk, not a foregone conclusion. As such, there are ways that you can prevent a herniated disc from developing, despite having scoliosis.
For instance, it’s important to maintain a healthy weight and engage in regular physical activity with scoliosis-specific exercises that won’t put too much strain on the spine. Doing so can have the following benefits:
- Strengthen the abdominal and back muscles to help support the spine
- Improve flexibility, balance, and posture
- Prevent further progression of the spinal curvature, thereby reducing the risk of herniation
In addition, it is vital to ensure that you use proper techniques when lifting heavy objects. If you have scoliosis, you should focus on maintaining a good posture and keeping a neutral spine when lifting heavy items, since there is a greater chance of herniating a disc during these types of movements.
Finally, you should also see a scoliosis specialist if you experience any sudden pain or muscle weakness in your back. Early diagnosis and treatment can help reduce the risk of disc herniation. With proper care, you should be able to minimize the risk of getting a herniated disc even if you have scoliosis.
How Do Scoliosis Specialists Diagnose Scoliosis And Disc Herniation?
A scoliosis specialist will typically perform a physical exam before ordering various imaging tests to diagnose scoliosis and a herniated disc. They will assess your posture, spinal alignment, and range of motion during the physical exam to determine if there are any signs of scoliosis or a herniated disc.
They might also ask you to perform certain movements or stretches. Doing so allows them to check for loss of reflexes, loss of sensation, muscle weakness, and pain, all of which may indicate a herniated disc. If they suspect scoliosis and/or a herniated disc, the specialist may also order some or all of the following imaging tests:
- X-rays: X-rays can provide detailed images of the spine and help specialists identify abnormal spinal curvatures, bone abnormalities, and the space between the bones (allowing them to identify potential herniated discs).
- Magnetic Resonance Imaging (MRI): MRIs use a magnetic field and radio waves to provide detailed images of the discs, nerves, and soft tissue in the spine. Scoliosis specialists will usually order an MRI if they suspect a herniated disc since x-rays can’t capture soft tissues (such as discs).
- Computerized Tomography (CT): CT scans take multiple x-ray images from different angles and combine them into a single image. Although an MRI is better suited for identifying herniated discs, CT scans give specialists a 3D image of the spine, allowing them to get a better view of any abnormalities in the spine.
- Electrodiagnostics: Electrodiagnostic tests use electrical stimulation to investigate the nerve pathways in the spine and measure electrical activity to determine if there is nerve damage. Scoliosis specialists will use electrodiagnostics if they suspect a herniated disc is causing nerve pain.
- Discography: Discography is a procedure where a special dye is injected into the discs to make them visible on an X-ray. This procedure can help scoliosis specialists identify the level of the disc herniation, allowing them to better target the treatment. Specialists will perform a discography to ensure they don’t target the wrong disc during a surgical procedure.
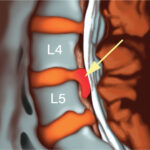
illustration of discography procedure of the spine
What Are The Treatment Options For People With Scoliosis And Herniated Discs?
If you have scoliosis and develop a herniated disc, there are a handful of treatment options available to help alleviate your symptoms. Whether or not the scoliosis specialist recommends an invasive procedure depends on the severity of your condition.
With that in mind, the following are a few of the potential treatment options available if you have scoliosis and a disc herniation:
Monitoring, Pain Medication, And Injections
When it comes to scoliosis and herniated discs, many doctors will monitor both conditions to determine if they progress or cause any additional issues. If the herniated disc does not cause significant changes in the spinal curvature or pain, then monitoring it is often the best option.
If you’re feeling mild pain due to the herniated disc, a traditional doctor may recommend hot or cold therapy. For moderate to severe symptoms, traditional doctors may prescribe medications such as non-steroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, painkillers, or steroid injections.
However, it’s essential to understand that general practitioners are not usually scoliosis experts. Scoliosis specialists will not recommend medications as they do not treat the underlying cause, only the symptoms – and the potential side effects of many of these medications can be problematic.
Instead, scoliosis specialists will likely prescribe scoliosis-based exercises and stretches tailored to the patient’s specific condition in order to prevent further progression and help correct the existing curvature.
Bracing
Bracing is a standard treatment method for scoliosis. It’s a non-invasive procedure that involves wearing a customized brace to help keep the spine in its correct position. This may be recommended for adolescents and children with scoliosis, as it can help reduce the progression of the condition by providing support and improved posture.
However, bracing can also be effective for scoliosis patients with herniated discs. A brace can help reduce the pain caused by a herniated disc by stabilizing the spine and, in some cases, help correct the spinal alignment and load distribution.
Physical Therapy
Physical therapy can be very beneficial to patients with scoliosis in general, as it can help strengthen the muscles around your spine and improve both flexibility and mobility. Certain stretches and exercises can also help if you have a herniated disc.
Physical therapy can help reduce pain by relieving the pressure on any of your nerves that may be compressed due to the herniated disc. There are also core exercises that you can do to stabilize the spine, which can help reduce the risk of further injury.
For most people, a combination of physical therapy, scoliosis-based exercises, and science-based chiropractic techniques can help manage the symptoms of a herniated disc effectively.
Non-Surgical Spinal Decompression
For more severe cases, a scoliosis specialist may recommend non-surgical spinal decompression. This treatment involves traction therapy with a special machine to gently stretch out the spine and decompress any affected discs.
This can help relieve any pressure placed on the nerves or muscles, reducing pain and inflammation. Specialists have used non-surgical spinal decompression to treat patients with scoliosis, herniated discs, or both of these conditions.
Corrective Surgery
If non-invasive treatment methods prove unsuccessful and you are still experiencing pain or discomfort, a specialist may suggest corrective surgery. However, corrective surgery is typically only recommended for severe pain or significant losses in mobility and range.
The following are some of the corrective surgeries that a scoliosis specialist might recommend for patients with severely herniated discs:
- Decompression Surgery: Also called a “laminectomy,” decompression surgery involves removing all or part of the lamina, which is the outer wall of the vertebrae that protect the spinal cord. This procedure can help relieve pressure on the spinal cord.
- Microdecompression: Also known as “microdiscectomy,” this procedure is one of the most common surgeries for herniated discs. The minimally invasive procedure involves removing a small portion of the herniated disc to help relieve the pressure on any affected nerves.
- Osteotomy: An osteotomy is a complex surgery that involves cutting, reshaping, and reinforcing the vertebrae to correct misalignment in the spine. It’s usually only recommended for patients with severe scoliosis or herniated discs.
- Spinal Fusion: Spinal fusion is an invasive surgery that involves fusing two or more vertebrae together, which helps reduce pain and improve stability in the spine by preventing further movement between the bones.
- Vertebral Column Resection: This surgery helps realign the spine by completely removing a vertebra from the vertebral column. A bone graft will be inserted in place of the removed vertebra. As it’s a complex surgery, it’s often only performed on patients if a previous surgery, such as an osteotomy, was unsuccessful.
As corrective surgery is invasive, it can take upwards of a year to fully recover. Not to mention, there are always risks involved with invasive surgeries of any kind, such as infection, nerve damage, and issues with anesthesia. Therefore, specialists will typically only recommend surgery as a last resort in cases of severe scoliosis and herniated discs.
Consult A Specialist, Consult With Square ONE Health
At Square One Health, our specialists can help diagnose and treat scoliosis before it leads to more serious conditions like herniated discs. If you are experiencing pain, numbness, or weakness from scoliosis or a herniated disc, our scoliosis specialists can help you find the right treatment plan that works for you.
Let Square ONE Health lead you to the path of recovery and a better quality of life. Schedule your free consultation today!